Antibiotic use in infants has been associated with a host of childhood conditions later in life. Yet when an infection is suspected in a newborn, usually a sample of their blood is drawn to check for the presence of bacteria and 5 to 8 percent of them receive antibiotics while the diagnosis is pending.
A team of researchers from Kaiser Permanente, the University of Pennsylvania, and the University of California, San Francisco has developed an infection risk calculator that clinicians can use to help them decide which infants to evaluate and treat for infection. The study, published in JAMA Pediatrics, and led by Michael Kuzniewicz, director of the Perinatal Research Unit at the Kaiser Permanente, reported that when the online calculator was utilized, antibiotic use declined to about 2.6 percent—with no increase in readmissions for undetected infections.
Solving the Problem of Group B Strep
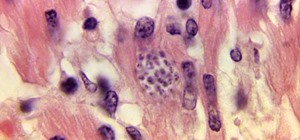
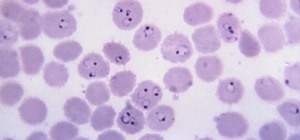
Exposure to bacteria from the mother's genital, gastrointestinal, and urinary tracts during the birth process can result in colonization of the baby with infectious organisms. One of the main causes of neonatal infections has been group B streptococcus.
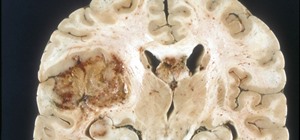
Infants infected with group B streptococcus have fever, difficulty feeding, irritability, or lethargy, but the most common symptom in a newborn is difficulty breathing. About 80 to 85 percent of the group B infections are in the babies' blood, 10 to 15 percent is pneumonia, and a brain infection—meningitis— accounts for 5 to 10 percent of the cases. Two to three out of every 50 babies who get a group B strep infections will die.
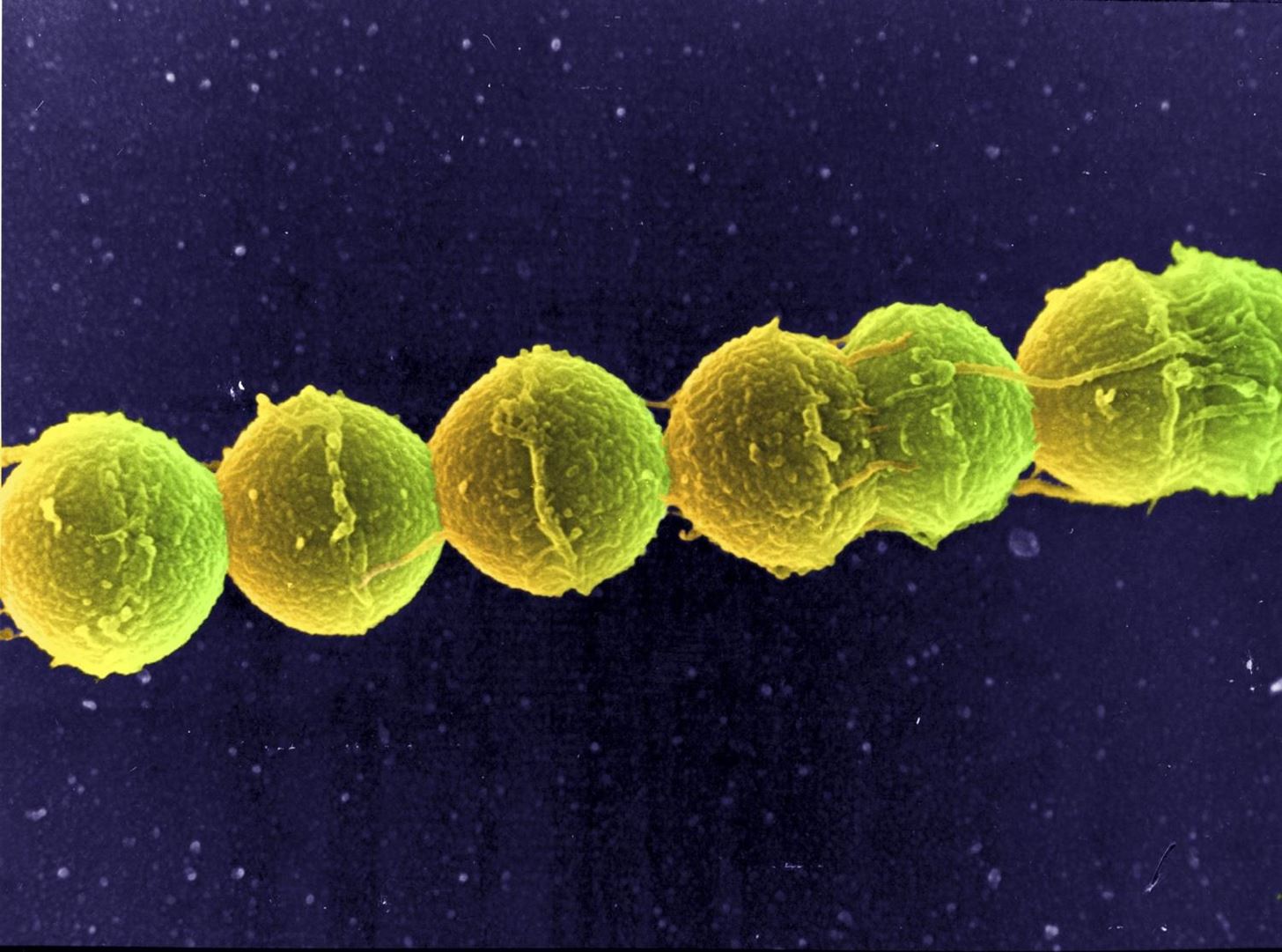
Presently, women with group B streptococcus infections—vaginal, gastrointestinal, or urinary—are treated during delivery with antibiotics. This has decreased the incidence of the infection in newborns from 1.7 cases per 1,000 live births in 1993 to 0.24 cases per 1,000 live births in 2014.
However, some newborns still get infected with the bacteria during birth. We know that this infection can be life-threatening in newborns, but we also know about the effects of early antibiotic treatment on a child's later health and how repeated antibiotic exposure contributes to the development of antibiotic-resistant bacteria.
To find a way to predict which babies might get the infection, the researchers developed a model using data from about 600,000 babies and their mothers who delivered at hospitals in Boston and at Kaiser Permanente facilities in Northern California. They created an algorithm to predict a newborn's probability of having an infection that combined data on gestational age, highest maternal temperature just after birth, whether the mother was a carrier of group B Streptococcus, time since rupture of membranes, and the nature and timing of antibiotics given during the birth, as well as information from examination of the infant.
When the infection prediction calculator was applied to 56,000 newborns, blood cultures to evaluate for infection declined 66 percent, from 14.4 to 4.9 percent. Antibiotic use declined 48 percent, from 5 to 2.6 percent.
Cutting More Than Antibiotic Use
Newborns treated with antibiotics have increased rates of childhood obesity, asthma, and pediatric inflammatory bowel disease, among others. A decrease in antibiotic use this early in life means one less healthcare test cost, one less blood draw, one less (potentially intravenous) medication for the baby, and can help decrease overall development of antibiotic-resistant bacteria.
"Instead of admission to the neonatal intensive care unit for intravenous treatment, the babies remain with their mothers, which improves bonding and the initiation of breastfeeding in the first days of life," coauthor Dr. Allen Fischer, of Kaiser Permanente, said in a press release.
The researchers emphasized that no antibiotic treatment was not the same as providing no care. Facilities that adopt the predictive model approach must ensure that other resources are available to provide access to pediatric care.
Use of the new risk calculator incorporates more variables into decision-making than clinicians currently use and strengthens the conclusion to treat or not treat. The result is a highly accurate model that can cut antibiotic use and might cut negative impacts on babies' later health.
Just updated your iPhone? You'll find new emoji, enhanced security, podcast transcripts, Apple Cash virtual numbers, and other useful features. There are even new additions hidden within Safari. Find out what's new and changed on your iPhone with the iOS 17.4 update.



















Be the First to Comment
Share Your Thoughts